Keeping up with doctor’s appointments is essential to managing health and staying informed, but it can often feel overwhelming. From scheduling and transportation to understanding medical advice and ensuring proper follow-up, there are many details to manage. This is where Understood Care can help. Our advocates serve as trusted guides, working alongside you or your loved one to make the process easier, more organized, and more comfortable.
Personalized Support Before and After Every Appointment
Understood Care advocates provide hands-on help with all aspects of medical visits. We help you schedule appointments, confirm provider information, and prepare for the visit itself. This might include reviewing your questions ahead of time, making sure prescriptions are current, or gathering any medical records needed. After the appointment, we help you understand the doctor’s recommendations and take the right steps to follow through on care instructions, referrals, or additional tests.
A Partner to Help You Understand Your Care
Medical visits can involve unfamiliar language, new diagnoses, or complex treatment plans. Your advocate is there to help translate this information into clear, understandable terms. We make sure you feel confident about what was discussed during the visit and that you know what actions to take next. If something is unclear or left unanswered, your advocate can follow up with your provider to get the information you need.
Coordination Across Your Care Team
Many people receive care from more than one doctor. Your advocate helps ensure that your care is well coordinated across primary care providers, specialists, and other professionals. We help share information between offices, keep records consistent, and make sure appointments align with your overall care goals. This reduces confusion and helps prevent important details from being overlooked.
Support for Getting to and From the Appointment
Transportation should never be the reason you miss a doctor’s visit. Your advocate helps you arrange reliable ways to get to and from appointments. Whether that means booking a ride service, coordinating with a caregiver, or finding community transportation resources, we make sure you have safe and timely access to care. We also consider mobility needs, language assistance, and other accessibility factors to support your comfort and safety.
Emotional and Practical Support Throughout
Doctor’s visits can bring up feelings of stress, uncertainty, or fatigue, especially when managing long-term conditions or complex health needs. Understood Care advocates are here to offer steady support throughout the experience. We are here to listen, provide encouragement, and help you make informed decisions without feeling overwhelmed.
Confidence in Every Step of the Journey
With Understood Care, you are never alone in managing your medical appointments. From the moment you schedule your visit to the follow-up that comes afterward, your advocate is there to help you stay organized, prepared, and empowered. We make it easier to stay connected to the care you need and to move forward with confidence.
Introduction
Grocery allowances, utility credits, and over the counter (OTC) allowances can be meaningful. They can also be confusing, especially when a plan changes names, eligibility rules, or how a benefit card works.
If you are trying to figure out whether your 2026 coverage includes one of these benefits, the safest approach is to rely on the official plan documents that control what is covered, not marketing language or what a friend’s plan includes. Medicare plans are expected to send key documents each fall that describe what will change in January.
Why grocery, utility, and OTC benefits can change every year
Medicare Advantage plans may offer supplemental benefits in addition to Original Medicare services. These benefits are set by each plan and can be added, redesigned, limited, or removed from one plan year to the next. Federal rules also allow plans to package benefits into an “allowance” model and, in some cases, deliver that allowance through a debit card or similar method.
Some grocery and utility benefits are offered as Special Supplemental Benefits for the Chronically Ill (SSBCI). These benefits can be targeted to members who meet the plan’s “chronically ill enrollee” criteria and the plan’s own eligibility rules. They are not automatically available to everyone in the plan, even when the plan advertises a flex card or allowance.
National reviews show that supplemental benefits are widespread but vary across plans, counties, and years, and federal reviewers note that utilization data for these benefits can be limited.
Peer reviewed analyses show that adoption of newer supplemental benefits varies across plans and years.
Some nonmedical benefits are designed as short term supports, for example posthospitalization home delivered meals. That is one reason it is important to confirm the exact duration and eligibility rules in your EOC.
Start with the two documents that control your 2026 coverage
Plan Annual Notice of Change (ANOC)
Your plan’s Annual Notice of Change explains what will change in January, including benefit additions, benefit removals, cost changes, or service area changes. Medicare.gov notes that the ANOC includes changes that will be effective in January and is sent each fall.
If you did not get an ANOC, treat that as a signal to contact the plan and request it. Medicare.gov specifically advises contacting your plan if you do not receive this document.
Evidence of Coverage (EOC)
Your Evidence of Coverage is the detailed rulebook for your plan year. Medicare.gov explains that the EOC gives details about what the plan covers, how much you pay, and more, and that it is sent each year, usually in the fall.
Summary of Benefits and benefit cards
Many plans also provide a Summary of Benefits and, in some cases, a benefit card. These can help you understand the basic idea of the benefit, but they may not show every restriction.
A card does not automatically mean you have a grocery, utility, or OTC benefit. The key detail is always the plan document language that defines what the allowance can be used for, who qualifies, and when funds reset or expire.

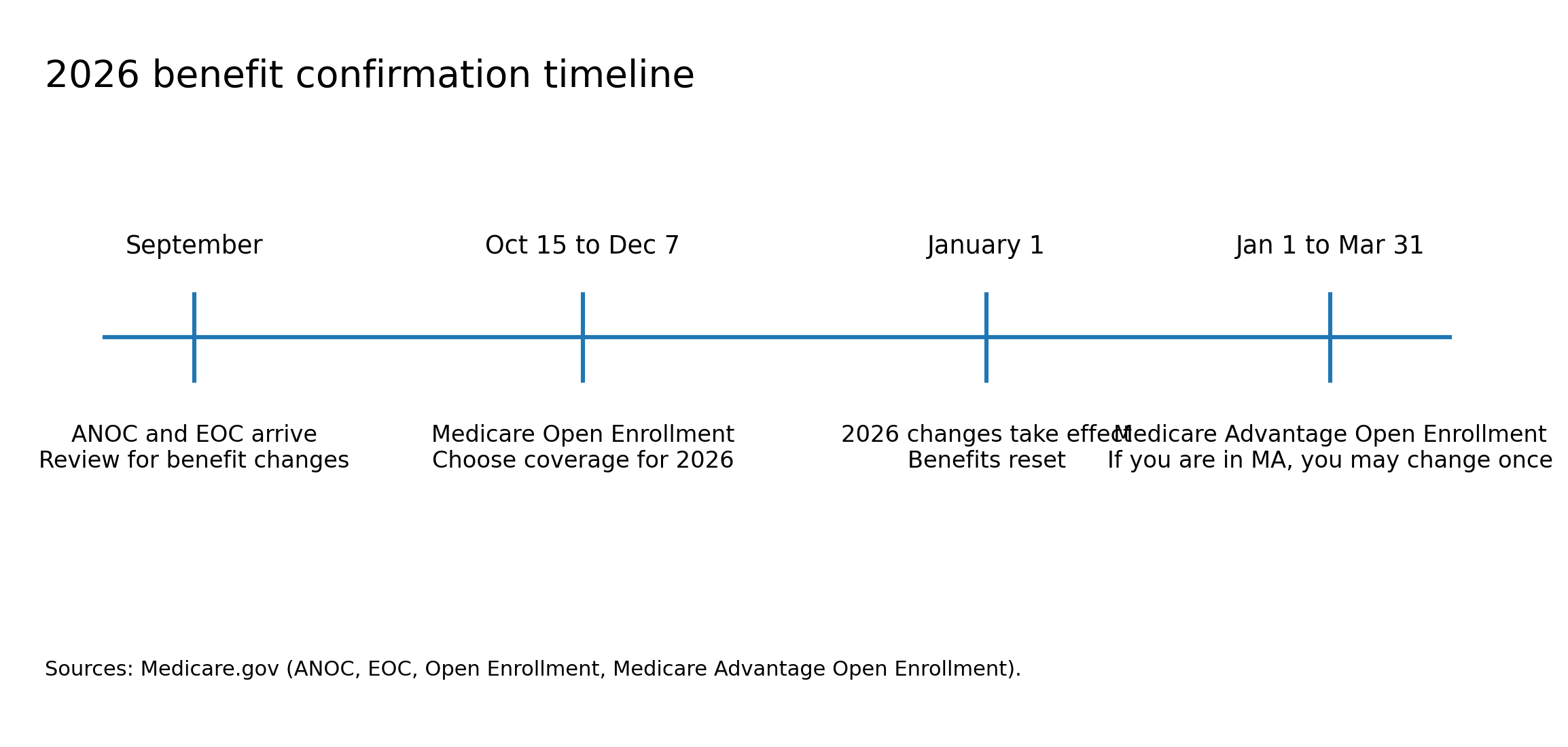
Key timing for reviewing 2026 benefit changes
Medicare plan changes described in your ANOC are generally effective in January, which is why it helps to review the ANOC and EOC as soon as you receive them.
Medicare’s official “Understanding Medicare Advantage Plans” booklet explains that plans notify you about changes through the Annual Notice of Change, and reviewing your documents early gives you time to confirm details before enrollment deadlines.
A step by step checklist to confirm grocery, utility, and OTC benefits for 2026
- Confirm you are looking at the right plan and the right year.
- Look at your member ID card and write down the plan name exactly as printed.
- If you have multiple cards in the household, confirm whose plan you are checking.
- On the ANOC or EOC, confirm it is for the 2026 plan year and that changes are effective in January.
- Find the benefit section in both the ANOC and the EOC.
- The ANOC tells you what changed.
- The EOC tells you the full rules.
- Use a keyword search inside the PDF.
- On a computer, open the PDF and use the “find” function.
- Search more than one term because plans use different labels.
- Helpful search terms include:
- OTC
- over the counter
- allowance
- flex
- food and produce
- healthy foods
- grocery
- utility
- general supports for living
- SSBCI
- chronically ill
- Confirm whether the benefit is available to all members or only certain members.
- If the benefit is described as SSBCI or tied to a “chronically ill enrollee” standard, it may require you to meet clinical criteria and additional plan criteria.
- If the benefit is described as an optional or mandatory supplemental benefit offered uniformly, it may be available to all members in that plan, but you still need to confirm any limits and conditions.
- Verify the allowance amount and the reset schedule.
- Look for whether the amount renews monthly, quarterly, or yearly.
- Look for whether unused funds roll over or expire.
- Plan allowances and reimbursements are generally tied to the plan year, which is one reason plans often treat these benefits as “use it within the plan year” benefits.
- Verify exactly what the benefit can be used for.
- Grocery and food benefits may be limited to certain categories of food, specific retailers, or a set list of eligible items.
- Utility benefits may be restricted to specific utility types or payment methods and may require you to submit bills or use an approved payment channel.
- OTC benefits often have a plan specific catalog or approved item list and may exclude items that seem “health related” to you but are not approved by the plan.
- Check whether you must take an extra step to activate or enroll.
- Some plans require activation, a separate enrollment step, or documentation to confirm you qualify for a targeted benefit.
- Look in the EOC for terms like “enrollment,” “activation,” “documentation,” or “prior approval.”
- If anything is unclear, ask for a written clarification.
- Call the member services number on the back of the card and ask them to point you to the page and section in the EOC that governs the benefit.
- If you are told you qualify, ask what documentation the plan used to make that determination and what could cause eligibility to change.
- If you are told you do not qualify, ask whether the plan offers the benefit only as SSBCI or under another limited category, and ask how the plan defines eligibility.
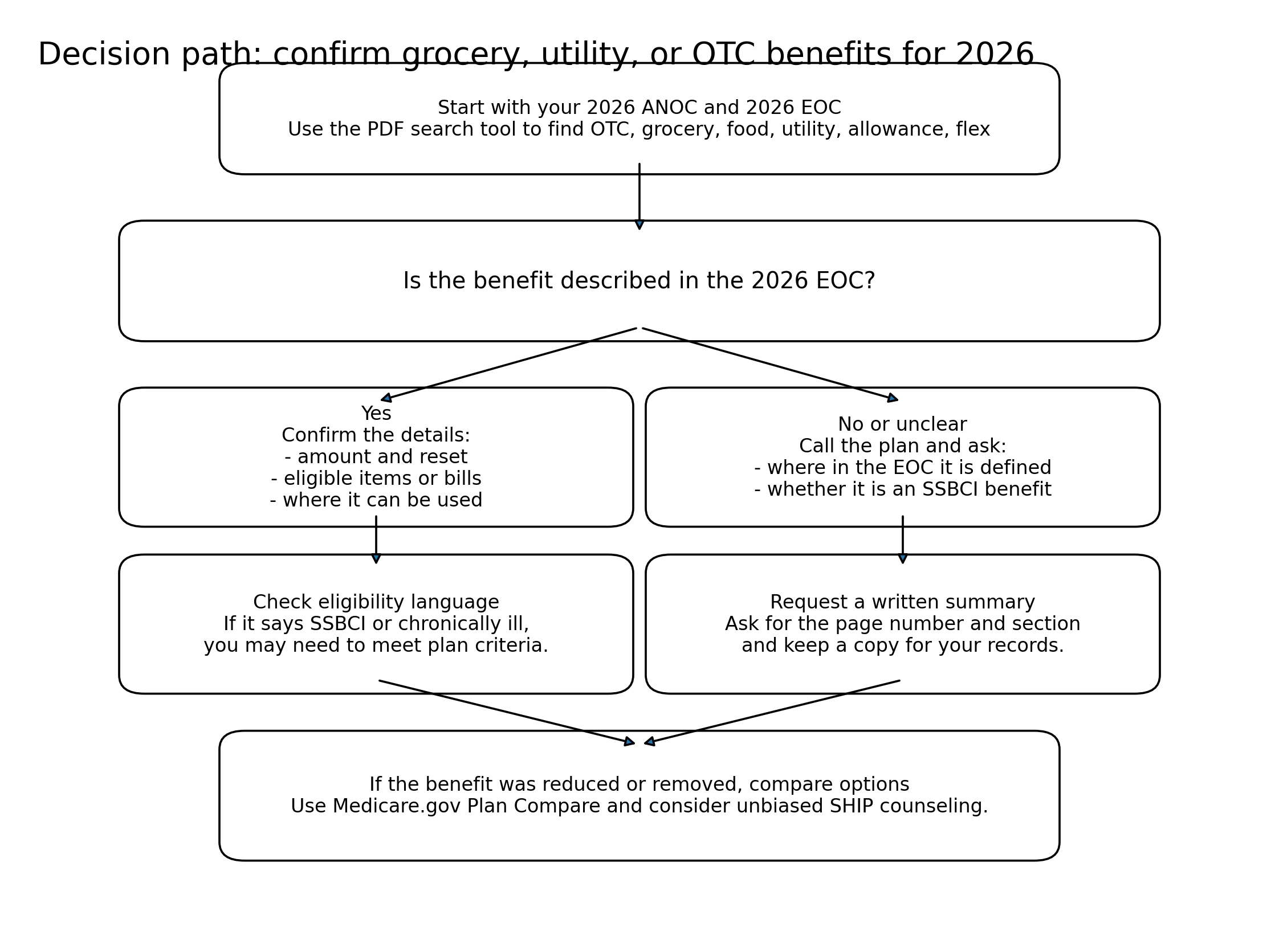
How to tell if a benefit was added or dropped for 2026
Use the ANOC as your quick comparison tool. Medicare.gov explains that the ANOC includes changes in coverage and costs that will be effective in January.
Then use the EOC to confirm what the change means in practice. Sometimes a benefit is not fully removed but is narrowed, for example, reduced dollars, fewer eligible items, a tighter eligibility definition, or a different schedule.
Red flags that usually mean you need a closer look
- You see the benefit mentioned in a flyer, but you cannot find it anywhere in the ANOC or EOC.
- The plan calls it a “flex” or “allowance” benefit, but the document does not clearly say groceries, utilities, or OTC are allowed uses.
- The benefit language includes SSBCI or “chronically ill enrollee,” but you have never been told you are enrolled in an SSBCI program or asked to confirm eligibility.
- A benefit card works at some stores but not others, or declines for items you thought were covered. This can happen when eligibility lists or item lists are narrower than expected.
If your 2026 plan dropped a benefit, practical next steps
If you relied on a grocery, utility, or OTC benefit and it was removed or reduced for 2026, you still have options. Start with confirmation, then move to replacement planning.
Confirm whether it was dropped for everyone or only for certain members
A plan may remove a benefit from a general package but keep a targeted version for certain members. SSBCI benefits can be limited to members who meet the plan’s criteria.
If you are a caregiver helping someone else, it can help to write down:
- The exact plan name
- The member’s Medicare number or member ID number
- A short description of the benefit you are trying to confirm, including the old amount and how it was used
Compare options using unbiased tools and counseling
Medicare’s official plan comparison tool can help you see plan options available where you live and compare benefits at a high level.
For free, unbiased help comparing plan choices, State Health Insurance Assistance Programs (SHIP) provide confidential counseling that is not connected to insurance companies.
Use plan by plan guides to speed up your short list
If you want faster starting points before you read full documents, Understood Care has plan by plan resources that can help you narrow what to check next:
- https://understoodcare.com/uc-articles/deep-plan-by-plan-comparisons-of-grocery-benefits
- https://understoodcare.com/uc-articles/which-medicare-advantage-plans-added-a-utility-allowance-for-2026-and-which-dropped-it
- https://understoodcare.com/uc-articles/how-advocates-help-you-find-your-best-health-plan
How Understood Care can support you
If you are managing this for yourself or someone you care for, the hardest part is often not finding information. It is knowing which details actually control eligibility and costs.
An Understood Care advocate can help you:
- Gather and organize the 2026 plan documents you need to make a clear decision
- Translate benefit language into plain steps, including what to ask the plan
- Track what the plan says in writing so you can avoid surprises later
- Build a simple “what changed” summary for your household
If you also need support with bills or paperwork, you can explore:
- https://understoodcare.com/uc-care-types/analyze-bills
- https://understoodcare.com/uc-care-types/utility-assistance
Related Reading
FAQ
- How do I check if my 2026 Medicare Advantage plan has an OTC benefit? Look in your 2026 ANOC for changes, then confirm the exact OTC allowance rules in the 2026 EOC, including eligible items and how the allowance renews.
- How can I confirm whether my plan added or dropped a grocery allowance for 2026? Search the 2026 ANOC and 2026 EOC for “food and produce,” “healthy foods,” or “grocery.” If it is not clearly listed in the EOC, assume it is not covered until the plan confirms it in writing.
- What is a Medicare utility allowance and how do I confirm it for 2026? Many utility allowances are described as a supplemental benefit or an SSBCI benefit. Confirm whether it is for all members or only for people who meet eligibility rules, and verify the payment method and covered utilities in your EOC.
- Why does my plan advertise a flex card but I cannot use it for groceries or utilities? “Flex” can mean different things. Your EOC should specify which categories are allowed uses. Some flex card programs are limited to OTC items or to targeted SSBCI benefits.
- Do SSBCI grocery or utility benefits apply to everyone in a plan? Not always. SSBCI benefits can be limited to members who meet the plan’s chronically ill criteria and the plan’s additional eligibility rules.
- What documents should I save to prove my 2026 benefit details? Save your 2026 ANOC, your 2026 EOC, and any written messages from the plan that confirm eligibility or the allowance amount.
- Where can I get free help checking 2026 Medicare grocery, utility, or OTC benefits? Your local State Health Insurance Assistance Program (SHIP) can help you review plan materials and compare options.
- If my 2026 plan dropped my OTC or grocery benefit, can I switch plans? You may be able to switch during applicable Medicare enrollment periods. Review your options early so you can compare benefits and costs before deadlines.
References
- https://www.medicare.gov/basics/forms-publications-mailings/mailings/costs-and-coverage/upcoming-plan-changes
- https://www.medicare.gov/basics/forms-publications-mailings/mailings/costs-and-coverage/evidence-of-coverage
- https://www.medicare.gov/plan-compare/
- https://www.medicare.gov/publications/10050-medicare-and-you.pdf
- https://www.medicare.gov/publications/12026-understanding-medicare-advantage-plans.pdf
- https://www.shiphelp.org/
- https://acl.gov/programs/connecting-people-services/state-health-insurance-assistance-program-ship
- https://www.cms.gov/medicare/health-plans/healthplansgeninfo/downloads/supplemental_benefits_chronically_ill_hpms_042419.pdf
- https://www.govinfo.gov/content/pkg/CFR-2023-title42-vol3/pdf/CFR-2023-title42-vol3-sec422-102.pdf
- https://www.gao.gov/assets/gao-23-105527.pdf
- https://www.medpac.gov/document/chapter-2-supplemental-benefits-in-medicare-advantage-june-2025-report/
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2819557
- https://jamanetwork.com/journals/jama-health-forum/fullarticle/2806411
- https://academic.oup.com/healthaffairsscholar/article/1/1/qxad019/7203737
Want a patient advocate by your side?
Quick & EasyMeet a supporting physician today for your 20-minute intake session.
Personal SupportAt Understood Care, you're seen, heard, and cared for.









.avif)
.avif)